Don't want to miss out on our latest updates?

Connecting data, technology and people, seamlessly
Connecting data, technology and people, seamlessly
Health knows no bounds. And neither should healthcare. At Philips, we believe there's always a way to make life better.
Health professionals:
How can we help?

Ultrasound imaging
Enhancing diagnostic confidence. Improving patient care
Solutions that are designed to help you confidently diagnose and care for your patients.
Cardiovascular care
Azurion 7 M20 in the Hybrid OR for vascular surgery
Sydney Adventist Hospital chose to partner with Philips to streamline their vascular procedures in the hybrid OR, the first Philips Azurion in ASEAN Pacific.

Healthcare services
Collaborating to drive healthcare transformation
Explore our range of strategic healthcare consulting to help you achieve clinical excellence and operational efficiency while improving financial performance and delivering quality patient care.
Cardiovascular care
Our cardiovascular care solutions help health systems meet the demands of a growing cardiovascular disease population inside and outside the hospital. Diagnostic innovations enable minimally invasive image-guided therapies, while integrated data and advanced informatics deliver a comprehensive view of a patient’s history. Patient monitoring solutions keep watch on the general ward and help detect patient deterioration earlier. Population health analytics help identify at-risk cardiac populations and ambulatory telehealth programs help monitor patients at home to reduce readmissions.
Monitoring
Our monitoring solutions go beyond measurements to address the broader challenges of health systems in keeping watch over patients continuously. Designed to enable virtually anywhere, anytime visibility into a patient’s condition, our patient monitoring products and clinical decision support tools deliver a more connected user experience while streamlining workflow with automated information flows. Our monitoring solutions integrate seamlessly into your IT infrastructure and deliver the data security you need.
Imaging
Our range of diagnostic imaging systems and software are designed to produce high quality images, improve efficiency and enable a better patient experience. From CT and MR to X-ray and ultrasound, our entire imaging portfolio aims to give care providers the right image at the right time, to support a faster, more confident diagnosis. Beyond the image, our imaging equipment includes advanced technologies that can increase repeatability while improving image clarity.
Healthcare informatics
Our healthcare informatics solutions aim to transform large amounts clinical data into integrated information that can help guide patient care throughout your enterprise. Our informatics solutions streamline management and analysis of patient data from imaging systems, patient monitors and cardiac testing equipment, while enhancing clinical pathways and aiding workflow. By connecting hospital information systems, you gain easy access to aggregated data across the patient care continuum, helping you to gain visibility into the overall health of a patient and proactively manage population health.
Clinical applications
To solve some of the most pressing clinical challenges in patient care, we offer a range of clinical applications that bring together hardware, software, technologies and services that can be tailored to meet your organization’s needs. From dose management to alarm fatigue, to integrated interventional therapies, we’ve designed solutions that help address clinical issues holistically by combining tools as well as the training, education and change management to deliver better outcomes.
Consulting & services
Our teams bring a deep expertise many aspects of healthcare, from clinical excellence, workflow optimization and patient experience, to equipment maintenance and staff training and education. Around your hospital and across your health system our people can enhance your operations, financial performance and care delivery to benefit staff experience and patient care. Day-to-day, we help keep you up and running, and operating at peak performance.
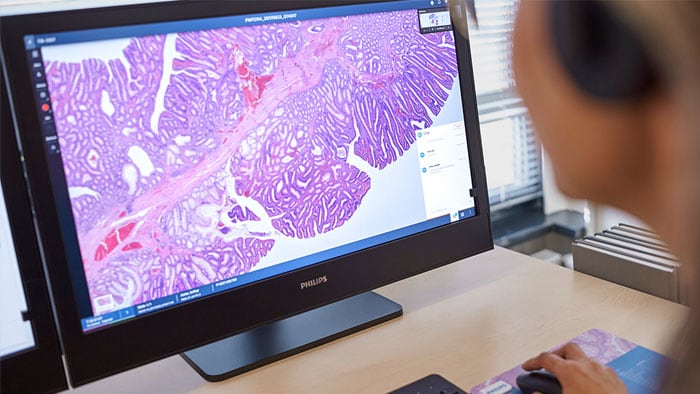
Diagnostic technologies
Digital advancements in healthcare hold great promise for improving diagnostic speed and confidence, as well as the most appropriate path for treatment. Our digital diagnostic solutions span analytics and informatics, and digital imagery and genomic data—all to enable a more informed and accurate patient-centric diagnosis.
Population health
Our population health management programs help drive quality improvement, revenue growth and business transformation for providers, health systems, employers and payers on a single, comprehensive platform. Our data platform aggregates patient data across networks and disparate systems and analyzes that data into a single, actionable patient record. Care management and patient activation programs helps health systems complete their transition to value-based care.